Clitoral pain and Interstitial Cystitis (IC) often coexist, creating a complex web of symptoms that can sometimes be difficult to unravel. Many doctors struggle to understand the complex relationship between interstitial cystitis symptoms and pelvic pain, resulting in frequent misdiagnoses.
In this article we will discuss the connection between interstitial cystitis and clitoral pain, providing insights into the causes, symptoms, and potential treatment options
By exploring the complexities of the body and examining the latest research, our goal is to make the understanding of how and why these conditions might be connected accessible to all.
What is Clitoral Pain?
Clitoral pain, also known as clitorodynia, is a specific form of pelvic discomfort that manifests as a sharp, stabbing, or burning feel in the clitoris. This discomfort is often experienced when the clitoris undergoes injury, infection, or damage, leading to symptoms such as burning, stinging, or throbbing.
The pain can be sporadic or constant, with intensity ranging from mild discomfort to severe pain that may disrupt your daily activities.
It is often worsened by activities that put pressure on the area, like sexual activity or wearing tight clothing. Clitoral pain is not a disease in itself, but rather a symptom of various underlying conditions, one of which is Interstitial Cystitis.
What does clitoral pain feel like?
Experiencing clitoral pain is a highly personal and unique journey that differs for each woman. For some, it may manifest as a lingering, dull ache, while for others, it can be an abrupt, sharp sensation that catches them off guard.
Some of the words used to describe clitoral pain are:
- Sensation of stinging or burning
- Throbbing or aching feeling
- Itchiness
- Sensation of stabbing or shooting
A woman named Jane who’s been dealing with clitoral pain and IC. She’s 35 years old and describes her pain as a “constant, intense burning sensation.” It burst out even with simple things like sitting for too long or just walking around.
This discomfort gets even worse during and after sexual intercourse. It turns something that should be intimate and enjoyable into a source of dread and anxiety. It’s just terrible how these conditions can really mess with your quality of life. It highlights the importance of effective treatment strategies and understanding medical care.
Possible causes of Clitoris pain
A painful clitoris can be caused by different factors. One common cause is the formation of keratin pearls, where the normal secretions of the clitoris turn into a hard, sand-like material. These secretions help the clitoral hood move freely, but keratin pearls hinder this movement, causing excessive rubbing and friction on the clitoris.
Other possible causes of clitoris pain are:
- Infections and diseases: Conditions like yeast infections, bacterial vaginosis, or sexually transmitted infections can cause clitoral pain, as can skin conditions like lichen sclerosus.
- Injury or Irritation: This can be caused by rough sexual activity, improper hygiene, or the use of aggressive soaps or detergents.
- Vulvodynia: A condition of chronic pain that affects the vulvar area, leading to clitoral discomfort.
- Interstitial Cystitis (IC): Chronic condition causing bladder pressure, pain, and sometimes pelvic discomfort. Pain severity can vary from mild to intense.
- Hormonal changes: Fluctuations in hormone levels during the menstrual cycle, pregnancy, or menopause can contribute to clitoral pain.
- Neuropathy: Damage to the pudendal nerve (which carries sensations from the clitoris) can result in pain.
- Psychological factors: Stress, anxiety, and depression can manifest as physical symptoms, including clitoral pain.
- Trauma to the area: Non-sexual trauma to the area may result from conditions like vaginal childbirth or surgical procedures.
- Sexually transmitted infections (STIs): A lot of the most common STIs can also cause clitoral pain.
To effectively treat and manage clitoral pain, it is important to understand its root cause. If you experience ongoing pain, it is recommended to consult a medical professional.
Also Read: Kidney Stone Pain in Clitoris: What Really Happens?
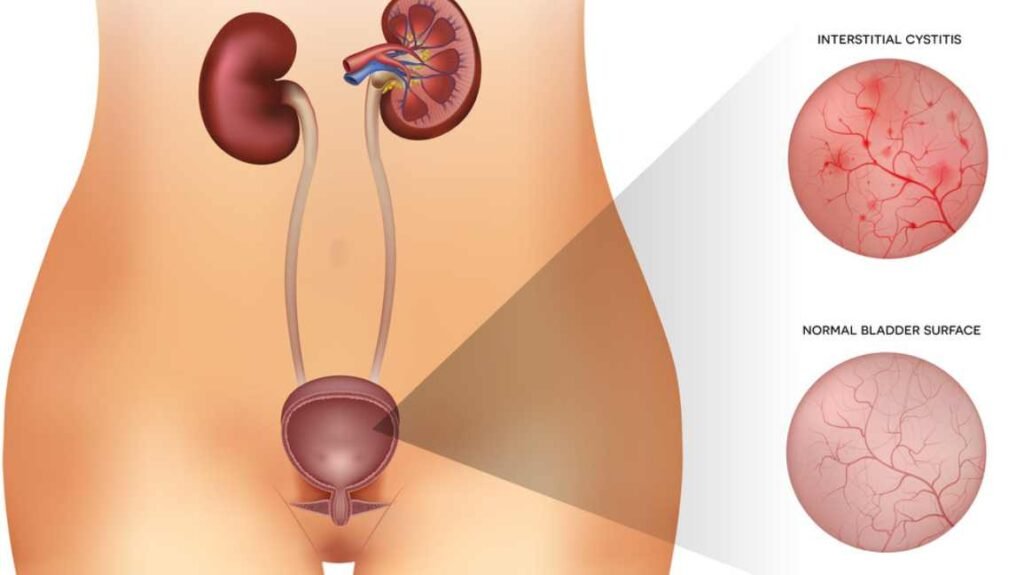
What is Interstitial Cystitis?
Interstitial Cystitis (IC), also refer as Painful Bladder Syndrome, is a long-term condition that causes discomfort in the bladder. It causes bladder pain and sometimes pelvic pain, ranging from mild unease to more intense discomfort. It is a part of a spectrum of diseases known as Chronic Pelvic Pain Syndrome.
This pain is commonly felt in the pelvic region, inguinal area, inner thighs, labia or vaginal lips, deep within the vagina, urethra, clitoris, and perineum.
The RAND IC Epidemiology (RICE) Study, the largest of its kind, suggests that approximately 3 to 8 million women in the United States (around 3% to 6% of all women) may suffer from IC.
There is no definitive cure for IC, but many treatments can offer relief. These may include medications, bladder instillations, nerve stimulation, physical therapy, and in severe cases, surgery.
Please remember, that if you experience bladder pain, frequent urination, or any other unusual symptoms, it’s important to consult with a healthcare provider.
Symptoms of Interstitial Cystitis
The symptoms of Interstitial Cystitis (IC) can vary greatly from one person to another but can include some or all of the following:
- Chronic pelvic pain or a persistent, pain pressure in the bladder area.
- intense pelvic pain (felt over your lower tummy)
- A frequent and urgent need to urinate, including frequent urination at night.
- Pain during sexual intercourse.
- Need to pee more often than usual.
- In women, symptoms often flare during menstruation.
- Pain or discomfort while the bladder fills, which is alleviated upon urination.
- In some cases, these symptoms may also be accompanied by lower back pain or discomfort in the lower abdomen.
Causes of Interstitial Cystitis
The exact cause of Interstitial Cystitis (IC) is unknown. Professionals believe that interstitial cystitis (IC) may result from a defect in the bladder’s protective lining, allowing harmful substances in urine to damage and inflame the bladder’s tissues.
Some people with IC may have a specific type of inflammatory cell, known as a mast cell, that releases histamine and other chemicals, causing IC symptoms.
Another theory suggests that certain elements, like autoimmune response, genetics, infection, or allergy, might contribute to the development of IC. For example, some people might have an inherited condition that affects the bladder or the body’s immune response.
Keep in mind that these are unproven factors that could play a role in Interstitial Cystitis.
The Connection: Clitoral Pain and Interstitial Cystitis
The connection between clitoral pain and Interstitial Cystitis (IC) is not immediately visible but it can be understood by considering the intricate network of nerves in the pelvic region.
The pudendal nerve, responsible for transmitting sensations from the clitoris, also provides innervation to the bladder and urethra. Therefore, inflammation or irritation in the bladder due to IC can potentially cause referred pain in the clitoris.
Women with IC often report increased sensitivity or pain in the clitoral and vulvar areas, pointing out a possible neural crosstalk between these regions.
Furthermore, the chronic pain and discomfort caused by IC can create a heightened state of tension and anxiety, affecting the body’s pain perception and response. This could make the clitoris and the surrounding areas more susceptible to pain or discomfort.
In contrast, clitoral pain may also be an independent occurrence due to other reasons mentioned earlier, such as infections, hormonal changes, or psychological factors.
Diagnosis and Treatment Options
Diagnosing Interstitial Cystitis (IC) can be challenging as symptoms often overlap with those of other common conditions like urinary tract infections, bladder infections, and endometriosis.
Diagnosis of interstitial cystitis might include:
- Medical history and bladder diary. You will be asked to keep a record of your urinary symptoms, fluid intake, and any pain or discomfort you experience in your bladder or pelvic region.
- Urinalysis. Your doctor may ask for a urine sample to check for signs of infection, traces of blood, or other abnormalities.
- Urinary cytology: This test examines the presence of abnormal cells that could suggest bladder cancer.
- Cystoscopy: A thin tube with a small camera is inserted through the urethra to view the lining of your bladder. Your healthcare provider may also inject liquid into your bladder to assess its capacity. This procedure, called hydrodistention, is typically performed after numbing you with an anesthetic medication to ensure your comfort.
- Biopsy. During cystoscopy, small tissue samples (biopsies) may be taken for laboratory analysis to rule out bladder cancer or other disorders.
- Potassium sensitivity test. In this test, the doctor fills your bladder with water mixed with different concentrations of potassium chloride. People with IC may have pain, urgency, or frequency during these tests.
- Pelvic exam. During a pelvic exam, your provider will assess your external genitals, vagina, and cervix. They will also palpate your abdomen to evaluate your internal pelvic organs. Additionally, they may also perform an examination of your anus and rectum.
Treatment
The treatment of Interstitial Cystitis (IC) focuses on alleviating symptoms and enhancing quality of life, as a permanent cure is yet to be found. Treatment strategies may differ, based on their symptoms and lifestyle.
- Lifestyle changes: Preliminary treatment strategies often involve lifestyle modifications like diet changes (avoiding food and drinks known to irritate the bladder), stress management, and exercises such as pelvic floor muscle training.
- Medication: Oral medications that may help manage IC symptoms include Nonsteroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants, and antihistamines. In some cases, doctors might recommend bladder instillations, which involve filling the bladder with a solution that includes a steroid and a local anesthetic.
- Physical therapy: Physical therapy can also be useful, especially for patients who experience pelvic floor dysfunction. A trained physical therapist can provide techniques for relaxation and pain relief.
- Surgery: In severe, unresponsive cases, surgery may be considered. However, it’s considered a last resort due to potential side effects and complications.
Common Questions from Women
Let’s answer some frequently asked questions by women about clitoral pain and interstitial cystitis to address common concerns.
My clit is swollen and in pain. What should I do?
If you’re experiencing clitoral swelling and pain, it’s important to consult with a doctor immediately. It could be an infection, allergic reaction or a more complex issue like Interstitial Cystitis.
During this, avoid any potential irritants like harsh soaps and wear breathable, cotton underwear. Also, refrain from any sexual activity that may exacerbate the discomfort until you’ve been seen by a healthcare professional.
Is clitoral pain common after menopause?
Yes, clitoral pain can be more common after menopause. This lower estrogen levels can cause vaginal tissue thinning and dryness, leading to discomfort during sex.
Decreased blood flow to this area may also contribute to sensory changes, including pain. Note that any persistent pain should be evaluated by your provider to rule out conditions like Interstitial Cystitis or other potential causes.
Can clitoral nerves be damaged?
Yes, the clitoral nerves can be damaged due to some reasons. This can include traumatic injury, surgeries in the pelvic region, or extensive bicycling that puts continuous pressure on the area. Damage to clitoral nerves can sometimes lead to sexual dysfunction or chronic pain, so early intervention is advised.
Do keratin pearls in the vulva cause clitoral pain?
Keratin pearls are hardened, keratinized skin cells that can form on the vulva, often as a result of skin conditions like lichen sclerosis. While keratin pearls themselves are not usually painful, the underlying condition causing them can cause discomfort, itching, and pain, including in the clitoral area.
Are keratin pearls dangerous?
Keratin pearls themselves are not dangerous. They are merely a physical manifestation of skin conditions, such as lichen sclerosus. However, the underlying condition causing them could potentially have serious implications if left untreated. In some cases, lichen sclerosus, for example, can increase the risk of skin cancer. Therefore, if you observe the formation of keratin pearls, it’s important to talk with your provider for proper diagnosis and management of the underlying condition.
Does Clitorodynia go away?
Yes, Clitorodynia, or pain in the clitoral area, can be resolved with the right diagnosis and treatment. However, the duration and success of the treatment largely depend on the hidden cause. Conditions causing Clitorodynia, such as nerve damage or infections, require specific treatments and the pain usually subsides once these conditions are appropriately managed. Over-the-counter pain relievers, topical anesthetics, pelvic physical therapy, or certain medications may help alleviate the symptoms.
Conclusion
Understanding the connection between clitoral pain and interstitial cystitis is important for those experiencing these symptoms. By seeking medical help, getting a proper diagnosis, and exploring suitable treatments can help manage and ease discomfort caused by these conditions. Remember every person has their own unique experience, and a doctor can provide personalized guidance and support. Don’t hesitate to reach out and prioritize your well-being.
Resources
- https://my.clevelandclinic.org/health/symptoms/23487-clitoris-pain-clitorodynia
- https://www.mayoclinic.org/diseases-conditions/interstitial-cystitis/diagnosis-treatment/drc-20354362
- https://www.nhs.uk/conditions/interstitial-cystitis/

Dr. Usman is a medical content reviewer with 12+ years of experience in healthcare research and patient education. He specializes in evidence-based health information, medications, and chronic health topics. His work is based on trusted medical sources and current clinical guidelines to ensure accuracy, transparency, and reliability. Content reviewed by Dr. Usman is for educational purposes and does not replace professional medical advice.
